Governor Proposes Cuts to Disability Services in May Revise Budget Proposal
Today, California Governor Gavin Newsom announced the May Revise of the 2025-26 state budget proposal. This budget proposal includes major cuts overall to Medicaid-funded services and DOES NOT include any potential impacts from the federal budget currently being considered in Congress. This means that the overall picture could get much worse in the next few weeks if the federal budget passes as currently proposed by the House of Representatives, which includes a $715 billion cut to Medicaid services. While we knew we were in a fight to protect Medicaid at the federal level, we did not expect we would also have a fight at the state level to protect Medicaid funded services, such as regional center services, Medi-Cal, In-Home Supportive Services (IHSS), and more.
Overall, the Governor’ May Revise budget anticipates a $12 billion shortfall next fiscal year and attributes the shortfall to both increased expenses in the state and decreased revenues due to President Trump’s tariffs and other economic policies. The budget proposal will now be considered by the Legislature, who will likely push back on certain parts of the Governor’s budget and will eventually send a final negotiated state budget back to the Governor by June 15. The massive federal cuts proposed by Congress, however, make the entire budget process more uncertain this year and may necessitate a second budget in the summer.
Below is a summary of several proposed cuts in the Governor’s May Revise budget that, if enacted, would impact California’s disability community:
DEVELOPMENTAL SERVICES
- Require Provider Mandates for Quality Incentive Program Eligibility—A reduction of $221.7 million General Fund in 2026-27 and ongoing associated with requiring compliance with Electronic Visit Verification, annual audits, and Home and Community-Based Services rules as a pre-condition of eligibility for the quality incentive component of the rate models.
- Health and Safety Waiver Assistance—A reduction of $3 million ongoing General Fund to eliminate health and safety waiver application assistance.
- Implicit Bias Training—A reduction of $5.6 million ongoing General Fund to eliminate dedicated resources for refreshing regional center implicit bias training.
- Direct Service Professional Workforce Training and Development (also known as “DSP University” or “DSP 1, 2, & 3)—A reduction of $17.6 million General Fund in 2025-26 and 2026-27, and $36.8 million General Fund in 2027-28 and ongoing to eliminate the Direct Services Professional Workforce Training and Development program, which has not yet been implemented.
- Self-Determination Program—A reduction of $22.5 million General Fund in 2025-26, and $45.5 million General Fund annually thereafter, to reflect new guardrails that will be imposed on individual spending budgets.
- Rate Reform Hold Harmless—A reduction of $75 million General Fund in 2025-26 to reflect ending the rate reform hold harmless policy in February 2026 instead of June 30, 2026. This means that service providers with rates above what is listed in the DDS rate models will have their rates reduced to match the DDS rate models in February instead of July.
MEDI-CAL
- Medi-Cal Asset Test Limits—Reinstatement of the Medi-Cal asset limit for seniors and disabled adults of $2,000 for an individual or $3,000 for a couple, effective no sooner than January 1, 2026. Estimated General Fund savings are $94 million in 2025-26, $540 million in 2026-27 and $791 million ongoing, inclusive of IHSS impacts. These asset limits were removed in 2024, meaning that a person could own more than $2000 in assets and still qualify for Medi-Cal. This proposal would reinstate those limits, meaning that if an individual owns more than $2000 in assets or if a couple owns more than $3000 in assets then they would not be eligible for Medi-Cal.
- Undocumented Individuals – Freeze enrollment into full-scope Medi-Cal, eliminate dental and IHSS benefits, and implement a $100/month premium. The last couple years California has made efforts to provide Medi-Cal coverage and other benefits to all Californians, regardless of documentation status. This proposal would walk that back and freeze any enrollment moving forward while allowing those already enrolled to maintain their Medi-Cal eligibility but with a $100/month cost. This proposal would also walk back other benefits, making undocumented individuals not eligible for IHSS, dental benefits, and other long-term care benefits.
SSI/SSP – No cuts, no increases.
IN-HOME SUPPOR SERVICES (IHSS)
- Cap IHSS provider overtime and travel hours at 50 hours per week beginning in 2025-26.
- Eliminate IHSS benefit for undocumented individuals.
- Those individuals who would no longer be eligible for Medi-Cal due to the Asset Test Limits would no longer be eligible for IHSS.
Click HERE to view and download the Budget Summary
WHAT’S NEXT?
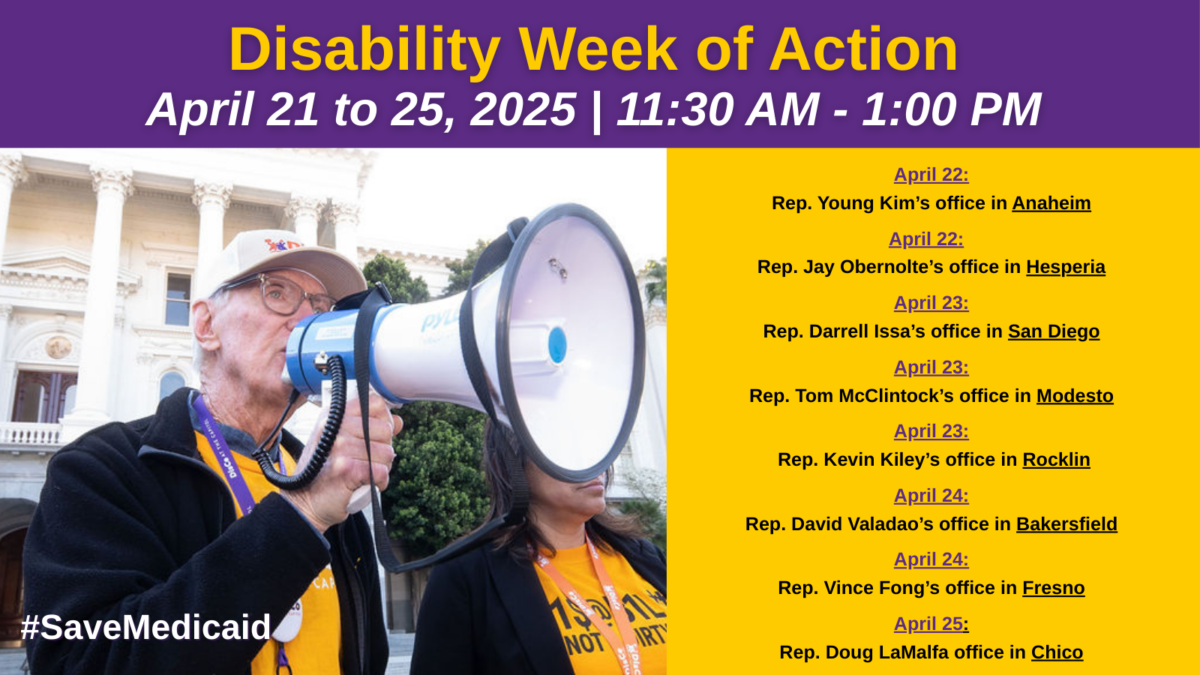
Our fight to protect vital disability services for Californians IS NOT OVER! We must continue to let our state and federal elected officials understand how devastating these proposed cuts will be to thousands of individuals with disabilities and their families. Click HERE to record a message that we can share.
Join us and organizations across the state for the Keep the Promise Rally on Thursday, May 22 at the California State Capitol in Sacramento from 11:30 a.m. to 1:00 p.m. to make our voices heard! Learn more at rally.thelantermancoalition.org